Backsliding - EOH 10/9

After several months of hope that New Yorkers were starting to leave lockdowns, New York’s leaders decided medieval lockdowns by neighborhood made good sense, specifically targeting Orthodox Jewish communities. New Yorkers rebelled and resisted the new street-by-street lockdowns. New York is not alone in its lockdown fetish, Israel is under an even more extreme lockdown, while deaths keep rising. Meanwhile in Europe, political leaders are avoiding lockdowns at all costs while cases rise dramatically but severe cases remain under control and at a much lower incidence than in the first quarter of this year.
Want to support our work? Visit our Substack page and leave us a tip.
On Rational Ground for our premium members, our data analyses will always be available to you and for general consumption and for public consumption. Additionally, for public consumption we released an update on how COVID-19 is like on university campuses.
COVID News
New York City’s Ultra-Orthodox Jewish Leaders Decry New Lockdown Measures
Freedom of religion is a right unless... COVID.
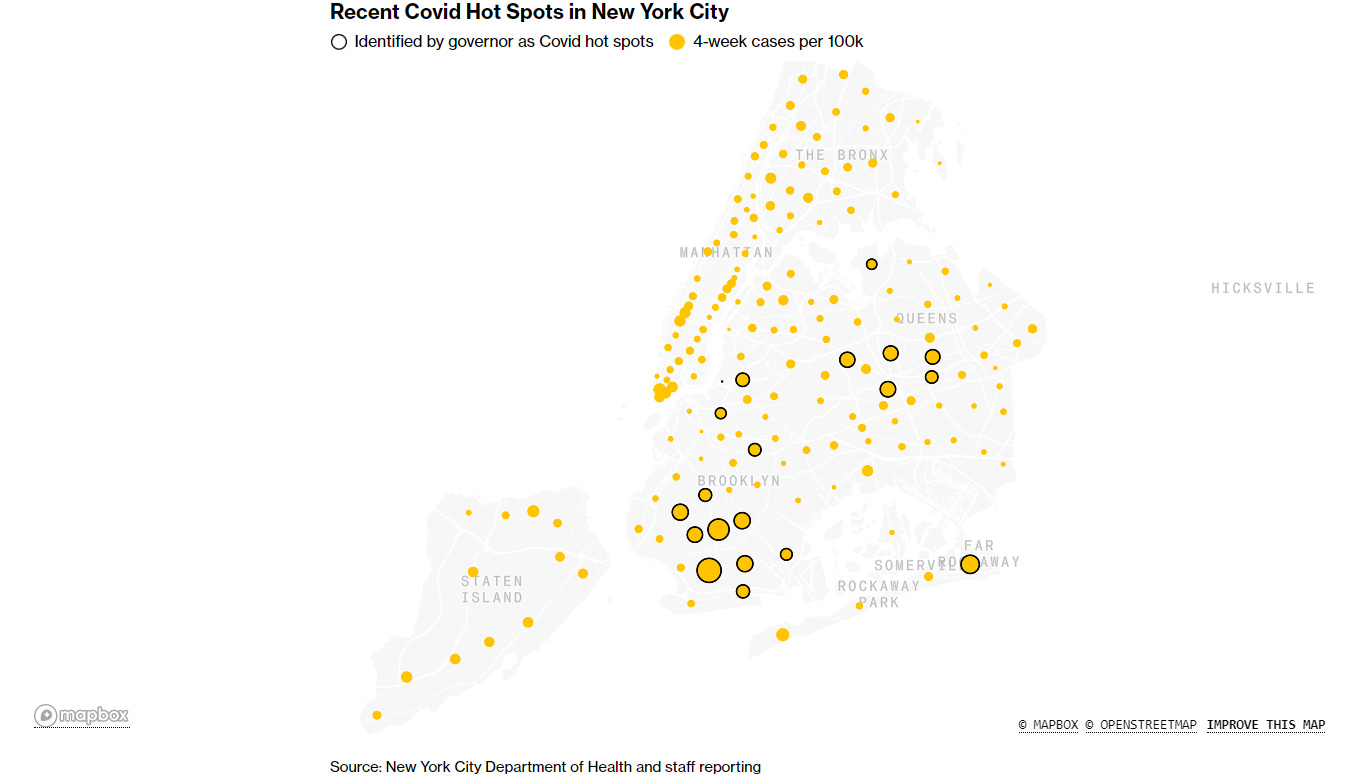
New York Gov. Andrew Cuomo’s order to lock down parts of the state seeing a resurgence of Covid-19 cases sparked protests and drew outrage from members of New York City’s ultra-Orthodox Jewish communities and their leaders. Under Mr. Cuomo’s order, some neighborhoods in Brooklyn and Queens, as well as parts of Rockland and Orange counties, must close schools and nonessential businesses, and limit religious gatherings to a maximum of 10 people. Many of the targeted areas have a high concentration of ultra-Orthodox Jews, who are in the middle of a religious holiday, Sukkot. The holiday is marked by gatherings and intermingling of large families. Dozens of ultra-Orthodox Jewish people in Borough Park, Brooklyn, protested Tuesday night, lighting a fire in a commercial street, according to New York Police Department officials and video shared on social media. The new lockdown measures come after city officials have for weeks tracked a surge in cases in nine ZIP Codes in Brooklyn and Queens. The transmission rate of Covid-19 in New York City remains low, at 1.65% over an average of seven days. However, in the nine city hot spots, the rate of people testing positive has been above 3% for at least seven consecutive days, Mayor Bill de Blasio has said. Mr. Cuomo said Tuesday that he had outlined his plan to Orthodox leaders ahead of his announcement and that it had been positively received. Agudath Israel of America, an umbrella group representing prominent ultra-Orthodox rabbis, described the plan as unanticipated and draconian. “It should be made clear that the Governor’s reference to a ‘good conversation’ he had earlier today with a group of Orthodox Jewish leaders was largely a one-way monologue, and contained no mention of this new plan,” the group said in a statement Tuesday evening.
Cuomo orders shutdowns in NYC’s COVID-19 hot spots
https://nypost.com/2020/10/06/cuomo-orders-shutdowns-in-covid-19-hit-areas-of-nyc/
Lockdown V2 in New York City by street. COVID knows street names and avenue numbers.
The heart of Brooklyn and two big swaths of Queens will again see non-essential businesses and schools shuttered by week’s end as the coronavirus surges in the city, Gov. Cuomo announced Tuesday. The edict came down following days of public back-and-forth between Cuomo and Mayor de Blasio, who on Sunday sought the state’s blessing to shutdown nine troubled ZIP codes in the boroughs. “When you see the cluster, you have to stop it at that point,” Cuomo said during an Albany press briefing. “Crush the cluster and stop the spread.” Cuomo on Monday granted de Blasio’s wish to close schools in the areas, but balked at locking up businesses until more precise lines of demarcation could be drawn than ZIP code borders. On Tuesday, he introduced a system guided by coronavirus diagnosis data and color-coded, with varying levels of restrictions in each zone. Red “intense clusters” will see all non-essential businesses and schools closed, restaurants reduced to takeout only, mass gatherings prohibited and houses of worship limited to a maximum of 25 percent capacity or 10 people, Cuomo said. The closures must be made no later than Friday — though a spokesman for de Blasio tweeted that they would likely begin Thursday — and run for at least two weeks. A map released by the governor’s office shows Brooklyn’s red zone encompassing a huge chunk of the borough, including much of Borough Park, Midwood and Homecrest.
California sees no link from school openings to virus spread
Surprise… not.
California has not seen a link between the reopening of K-12 schools for in-person learning and increased coronavirus transmission, the state's top public health official said Tuesday. Dr. Mark Ghaly, the state's Health and Human Services secretary, told reporters that officials have been closely watching the return to classrooms in counties where it has been allowed. He said it can take time for trends to emerge, but so far, the results are encouraging. “We have not seen a connection between increased transmission and school reopening or in-person learning,” Ghaly said. “We’re looking at the information to see if there is a connection, and so far we have not found one.”California requires counties to report coronavirus levels and infection rates below certain thresholds before they can allow K-12 schools to broadly reopen for in-person instruction. On Tuesday, 32 of the state's 58 counties were deemed eligible to do so — up from 28 a week earlier. Counties must meet the threshold for at least two weeks before schools are allowed to reopen. Yuba County, about 140 miles northeast of San Francisco, met the threshold for the first time on Tuesday. The county is preparing to reopen schools by limiting the number of students in each classroom to make sure people can stay at least 6 feet (1.8 meters) away from each other, Yuba County Superintendent of Schools Francisco Reveles said. Reveles said students would likely come to school in groups, with some groups attending in the morning while others attend in the afternoon. “We’re in a different environment now,” he said. “Even though we can open up, there’s certain precautions we need to continue taking.” The state has seen a broad decline in the number of coronavirus cases and hospitalizations in recent weeks. While some areas are seeing an increase in infections, the state's overall case numbers have fallen since a surge over the summer following the initial reopening of various business sectors.
We’ve Destroyed the Arts
https://bookandfilmglobe.com/creators/weve-destroyed-the-arts/
American culture is another victim of the lockdowns.
A quick scan of the performing arts listings reveals that the following events are going on in the United States this week: A performance of Sweeney Todd in St. George, Utah, a performance of “Blink: The Musical”, in Provo, Utah, and an outdoor performance of Handel’s “Water Music” by the Salt Lake City Symphony. So, relatively, Utah looks pretty good. As for the rest of the country, we have a passel of shows in Branson, Missouri, including the Dolly Parton Stampede, a socially-distanced concert by a Fleetwood Mac tribute band in Atlanta, a trio of Jason Isbell shows in suburban Nashville, and the Grand Ole Opry. That’s it. That’s the Arts in America. Maybe I’m missing something. Perhaps a lone guitarist is strumming out Bob Seger’s greatest hits to a small audience of drunken bikers in darkest Tucson. Maybe some hippie banjo player is entertaining a couple of dozen in a park in Manitou Springs. There might be a hip-hop speakeasy in Houston. But the fact remains: It’s not much. October is typically the liveliest cultural month of the year in this country, the former cultural capital of the world. But no more. Now we have nothing but reality TV, politics, disease, and charity celebrity Zoom readings of 80s teen comedies. We’ve destroyed the performing arts in America. Congratulations. Good job to all of us. There’s no public singing, dancing, speaking, or otherwise emoting. Coronavirus may continue to spread, but the arts are gone.
Stats Hold a Surprise: Lockdowns May Have Had Little Effect on COVID-19 Spread
Surprise if you weren’t paying attention.
In 1932, Supreme Court justice Louis Brandeis famously called the states “laboratories of democracy.” Different states can test out different policies, and they can learn from each other. That proved true in 2020. Governors in different states responded to the COVID-19 pandemic at different times and in different ways. Some states, such as California, ordered sweeping shutdowns. Others, such as Florida, took a more targeted approach. Still others, such as South Dakota, dispensed information but had no lockdowns at all. As a result, we can now compare outcomes in different states, to test the question no one wants to ask: Did the lockdowns make a difference? If lockdowns really altered the course of this pandemic, then coronavirus case counts should have clearly dropped whenever and wherever lockdowns took place. The effect should have been obvious, though with a time lag. It takes time for new coronavirus infections to be officially counted, so we would expect the numbers to plummet as soon as the waiting time was over. How long? New infections should drop on day one and be noticed about ten or eleven days from the beginning of the lockdown. By day six, the number of people with first symptoms of infection should plummet (six days is the average time for symptoms to appear). By day nine or ten, far fewer people would be heading to doctors with worsening symptoms. If COVID-19 tests were performed right away, we would expect the positives to drop clearly on day ten or eleven (assuming quick turnarounds on tests). To judge from the evidence, the answer is clear: Mandated lockdowns had little effect on the spread of the coronavirus. The charts below show the daily case curves for the United States as a whole and for thirteen U.S. states. As in almost every country, we consistently see a steep climb as the virus spreads, followed by a transition (marked by the gray circles) to a flatter curve. At some point, the curves always slope downward, though this wasn’t obvious for all states until the summer.
Research
Eli Lilly says its monoclonal antibody cocktail is effective in treating Covid-19
https://www.statnews.com/2020/10/07/eli-lilly-monoclonal-antibody-cocktail-covid-19/
The data does look good.
Eli Lilly said Wednesday a monoclonal antibody treatment is effective in reducing levels of the virus that causes Covid-19 in patients, and also appears to prevent patients from visiting the emergency room or hospital. Lilly had previously released results for a similar treatment using one antibody, which experts viewed as promising. But the new results, of a combination of two antibodies, appear, based on limited data provided in a press release, to be more robust. The results also appear roughly similar to those Regeneron presented last week of its own cocktail of two monoclonal antibodies. Last Friday, President Trump was treated with the Regeneron monoclonal antibodies. Monoclonal antibodies are synthetic versions of the antibodies that are one of the main weapons of the immune system. Researchers believed that injecting them into patients could help treat them. The patients in the study were sick with Covid-19, but had not been admitted to the hospital. Eli Lilly said that in a preliminary analysis the antibody combination reduced the amount of virus in nasal swabs of patients after 11 days. Key data, including the actual viral loads of patients and the makeup of the study population, were not included in the press release. In the study, 112 patients received 2.8 grams of each of the antibodies, and 156 received placebo. The difference in viral load was statistically significant at day 11, unlike some doses of Lilly’s single-antibody cocktail. There was also a statistically significant reduction in viral levels three days and seven days after infection. The treatment also improved symptoms, according to a scored questionnaire, and resulted in fewer hospital and emergency room visits. Visits to the hospital or ER were made by 5.8% of patients in the placebo group, but just 0.9% of those who received the antibody combination. That difference, however, was just barely statistically significant.
A Cost/Benefit Analysis of Clinical Trial Designs for COVID-19 Vaccine Candidates
https://www.nber.org/papers/w27882.pdf
An analysis on how to most efficiently design COVID-19 vaccine trials.
The COVID-19 pandemic has caused the deaths of hundreds of thousands, upended the lives of billions, and caused trillions of dollars in economic loss, and life is unlikely to return to normal until a vaccine is found. Despite the many candidates undergoing testing, an approved vaccine is not expected until 2021, even with substantially compressed development timelines, smooth proceeding of clinical trials, and not accounting for possible failures. It is possible—though considered highly unlikely at the present time—that, like many non-influenza epidemics, the crisis may be over before a successful vaccine is developed. Unlike typical therapeutics that are administered to sick patients, vaccines are intended for the healthy. Therefore, confirming the safety and effectiveness of a vaccine is of critical importance. The two primary methods for demonstrating vaccine safety and efficacy are through either a vaccine efficacy randomized clinical trial (RCT) or a vaccine immunogenicity RCT. In the former, large numbers of recruited healthy volunteers are randomly selected to receive either the vaccine or a placebo/active control and then monitored for a period of time. At the end of the surveillance period, the difference in the proportion of infections between the treatment and control arms is computed to demonstrate the ability of the vaccine to prevent infection or disease. A phase 3 vaccine efficacy RCT typically takes five to ten years to complete.
Face masks: what the data say
https://www.nature.com/articles/d41586-020-02801-8
Data about masks.
When her Danish colleagues first suggested distributing protective cloth face masks to people in Guinea-Bissau to stem the spread of the coronavirus, Christine Benn wasn’t so sure. “I said, ‘Yeah, that might be good, but there’s limited data on whether face masks are actually effective,’” says Benn, a global-health researcher at the University of Southern Denmark in Copenhagen, who for decades has co-led public-health campaigns in the West African country, one of the world’s poorest. That was in March. But by July, Benn and her team had worked out how to possibly provide some needed data on masks, and hopefully help people in Guinea-Bissau. They distributed thousands of locally produced cloth face coverings to people as part of a randomized controlled trial that might be the world’s largest test of masks’ effectiveness against the spread of COVID-19. Face masks are the ubiquitous symbol of a pandemic that has sickened 35 million people and killed more than 1 million. In hospitals and other health-care facilities, the use of medical-grade masks clearly cuts down transmission of the SARS-CoV-2 virus. But for the variety of masks in use by the public, the data are messy, disparate and often hastily assembled. Add to that a divisive political discourse that included a US president disparaging their use, just days before being diagnosed with COVID-19 himself. “People looking at the evidence are understanding it differently,” says Baruch Fischhoff, a psychologist at Carnegie Mellon University in Pittsburgh, Pennsylvania, who specializes in public policy. “It’s legitimately confusing.”
Charts and Graphics
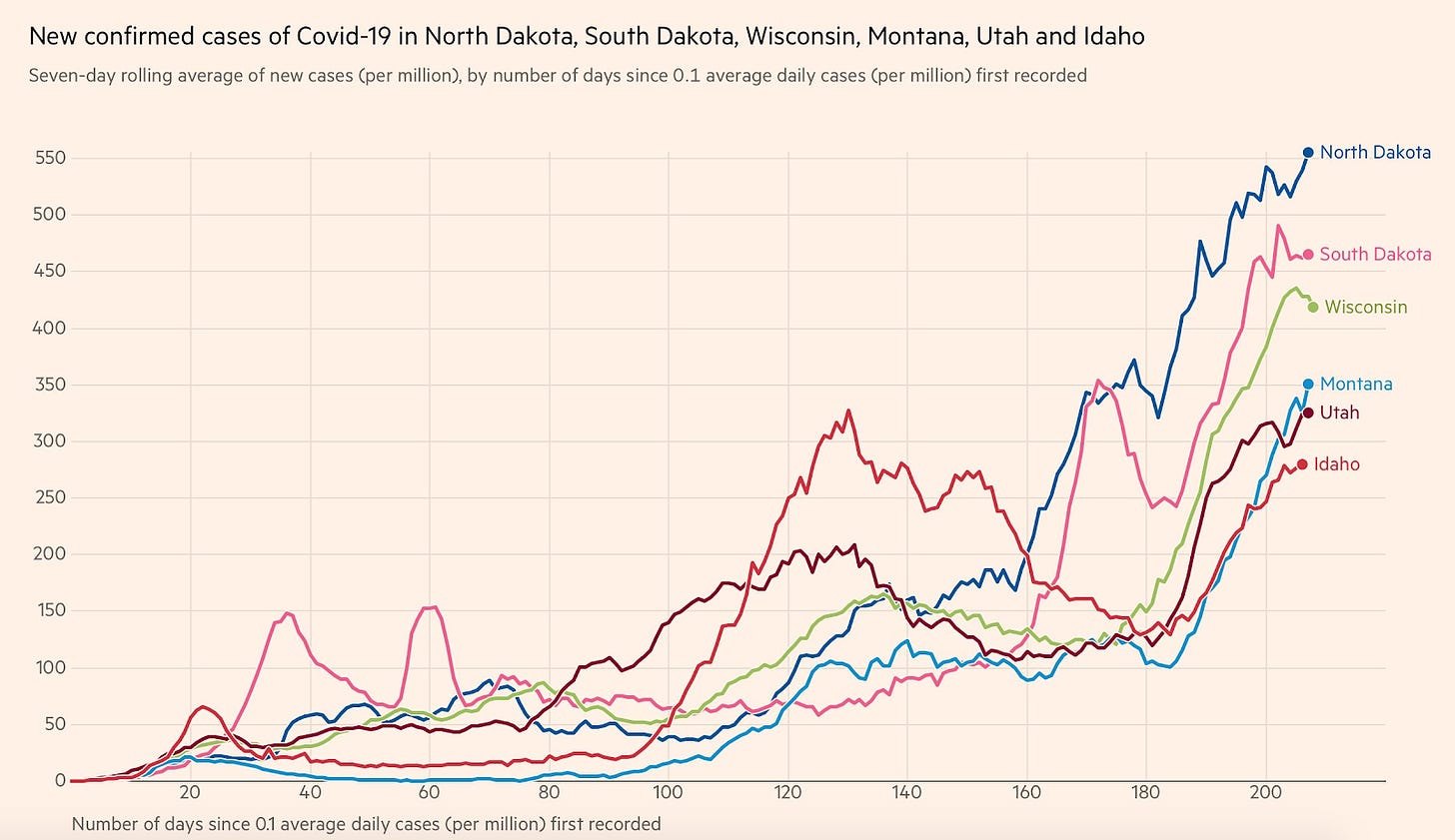
New Confirmed Cases of COVID-19 in North Dakota, South Dakota, Wisconsin, Montana, Utah, and Idaho
Cases rise in low incidence states, as expected.
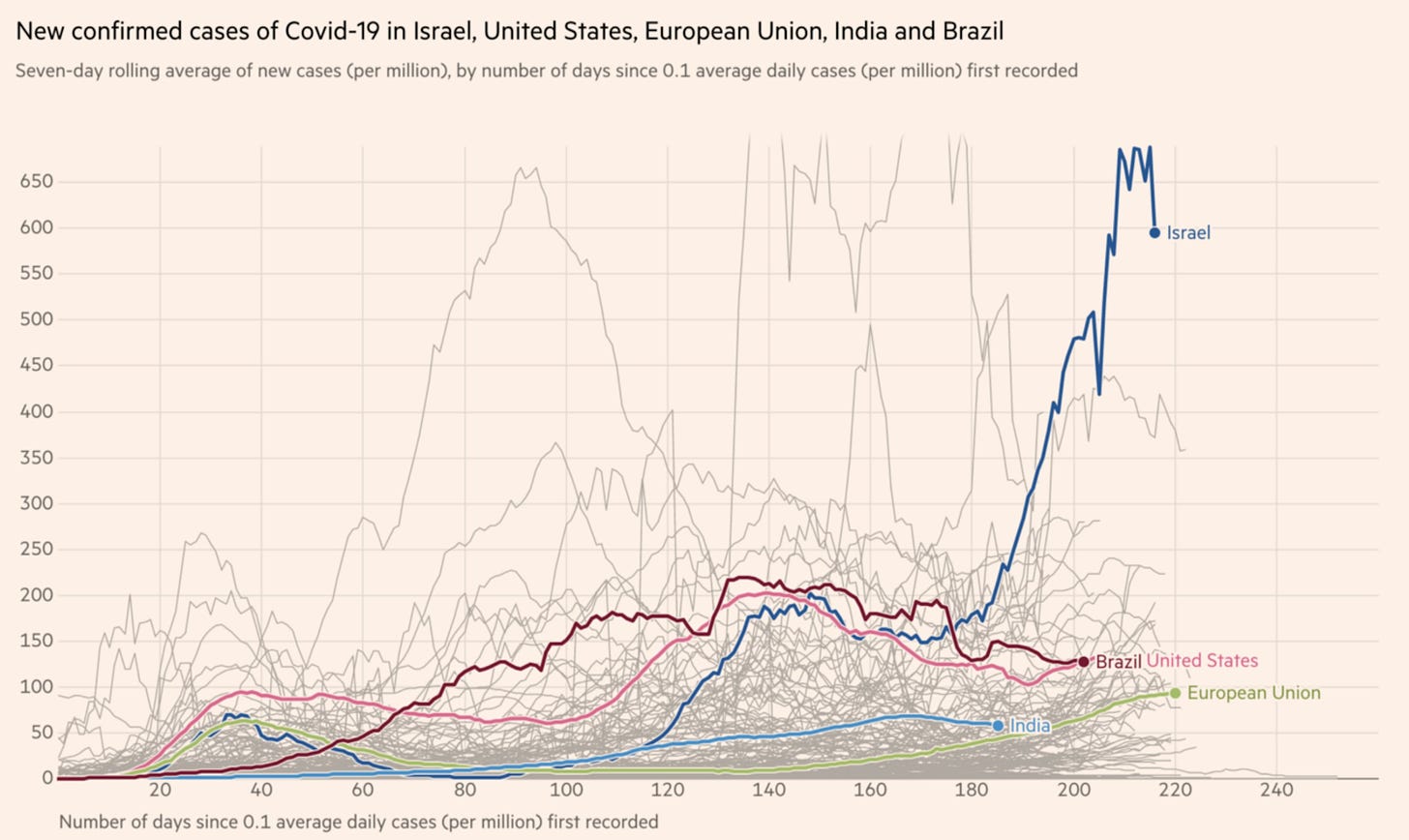
New Confirmed Cases of COVID-19 in Israel, United States, European Union, India and Brazil
How did lockdown-loving Israel handle COVID?
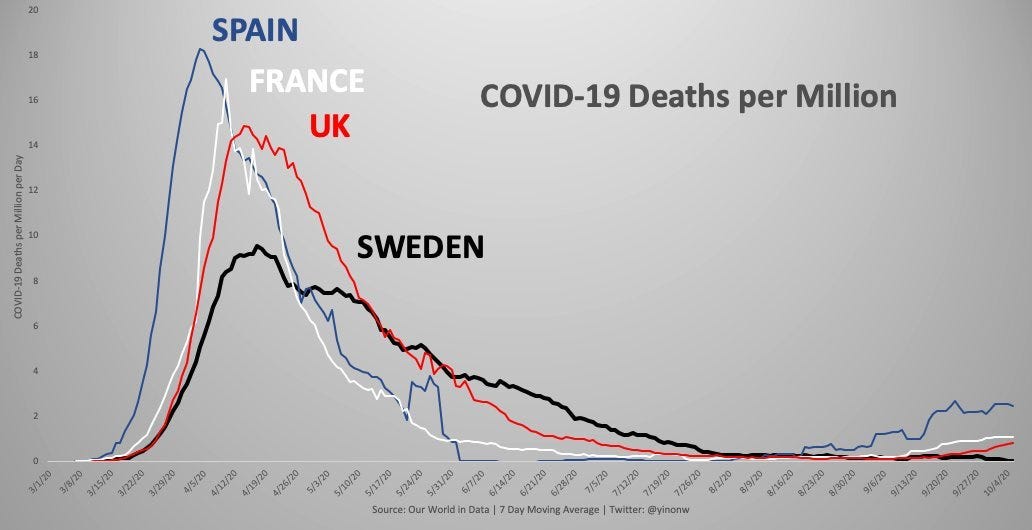
COVID-19 Deaths per Million (Spain, France, UK, Sweden)
Can you see Sweden’s second wave?
Recent COVID Hotspots in New York City
Hotspot mapping in New York
International News
The Great Barrington Declaration
An anti-lockdown manifesto by global health professionals
As infectious disease epidemiologists and public health scientists we have grave concerns about the damaging physical and mental health impacts of the prevailing COVID-19 policies, and recommend an approach we call Focused Protection. Coming from both the left and right, and around the world, we have devoted our careers to protecting people. Current lockdown policies are producing devastating effects on short and long-term public health. The results (to name a few) include lower childhood vaccination rates, worsening cardiovascular disease outcomes, fewer cancer screenings and deteriorating mental health – leading to greater excess mortality in years to come, with the working class and younger members of society carrying the heaviest burden. Keeping students out of school is a grave injustice. Keeping these measures in place until a vaccine is available will cause irreparable damage, with the underprivileged disproportionately harmed. Fortunately, our understanding of the virus is growing. We know that vulnerability to death from COVID-19 is more than a thousand-fold higher in the old and infirm than the young. Indeed, for children, COVID-19 is less dangerous than many other harms, including influenza. As immunity builds in the population, the risk of infection to all – including the vulnerable – falls. We know that all populations will eventually reach herd immunity – i.e. the point at which the rate of new infections is stable – and that this can be assisted by (but is not dependent upon) a vaccine. Our goal should therefore be to minimize mortality and social harm until we reach herd immunity. The most compassionate approach that balances the risks and benefits of reaching herd immunity, is to allow those who are at minimal risk of death to live their lives normally to build up immunity to the virus through natural infection, while better protecting those who are at highest risk. We call this Focused Protection.
Airlines hope Covid-19 health pass will have passengers flying again
https://www.ft.com/content/8d603248-6884-4081-9256-8c5b2f2827ba
Once temporary restrictions on freedom will soon become permanent.
The first trials of a digital health pass that certifies airline passengers are Covid-free will begin this week in a push to reopen international travel fully after nearly nine months of disruption. The World Economic Forum-backed CommonPass project aims to create the first globally recognised proof that a passenger has tested negative for the virus before a flight, using a digital certificate downloaded to a mobile phone. CommonPass will not conduct tests. Instead it aims to establish standard certifications for Covid-19 test results and, eventually, proof that a passenger has been vaccinated against the virus. Steve Morrissey, a regulatory and policy executive at United Airlines, which is part of the pilot scheme, said the trials were “critical” to developing an alternative to the quarantine requirements and travel restrictions currently in force in many countries. United and Cathay Pacific Airways are set to begin testing the digital health pass on routes linking travel hubs including London, New York, Hong Kong and Singapore on Thursday. The aviation industry is hopeful that passenger testing can restart international travel but many governments, including the UK’s, have stuck to blunt measures such as self-isolation requirements for incoming passengers. UK cabinet ministers, for example, have promised an announcement on airport testing, although industry executives expect any measures would only shorten the quarantine period. Etihad’s chief executive, Tony Douglas, told the Financial Times last month that health visas would be preferable to the so-called air corridors employed by some countries, including the UK, which he dismissed as a “marketing exercise”.
The pandemic’s shadow harvest: Will the economic and psychological costs of covid-19 increase suicides?
A worldwide tragedy that was preventable.
WHEN AMERICA’S Centres for Disease Control and Prevention (CDC) carried out a survey this summer, it found that one in ten of the 5,400 respondents had seriously considered suicide in the previous month—about twice as many who had thought of taking their lives in 2018. For young adults, aged 18 to 24, the proportion was an astonishing one in four. The survey, published in August, was one of a growing number of warnings about the toll that the pandemic is taking on the mental health of people. For legions, the coronavirus has upended or outright eliminated work, schooling and religious services. On top of that, lockdowns and other types of social distancing have aggravated loneliness and depression for many. But are people acting on suicidal thoughts? It is too early to be sure. Almost all countries publish suicide statistics with a lag of a year or two; and in recent years, suicide has been declining in most, with America a notable exception. Information from police, hospitals, coroners, courts and others must be collected and carefully studied, in part because some families report events selectively, or untruthfully, in the hope that a loved one’s probable suicide will be ruled a natural or accidental death. A comprehensive picture of suicide in the time of covid-19 has therefore yet to emerge. But experts have reasons to fear the worst. For one thing, calls to suicide hotlines are up. Some in America have seen volume multiply eight-fold, says Sally Curtin, a suicide expert at CDC. The number of young people seeking help has risen, as has the proportion in extreme distress, notes Brenda Scofield, chairwoman of Samaritans, a hotline charity, in Hong Kong. Talkspace, a New York firm that provides online therapy, says that video sessions have increased by 250% during the pandemic. The number of patients with severe anxiety is up by 40%, a leap unprecedented in Talkspace’s nine years of business. Neil Leibowitz, its chief medical officer, expects this to translate into what he euphemistically calls “a lot of downstream effects”. A few preliminary estimates of suicides during the pandemic have emerged. Though the figures will be revised, they bode ill. An initial tally of suicides in Japan in August put the number at 1,849, a jump of 15.3% over the same period last year, the health ministry has reported. Nepal’s national police force has said suicides during the pandemic seem to have climbed by a fifth. Thailand’s health ministry fears that nearly nine out of every 100,000 Thais will have killed themselves this year, up from 6.6 in 2019, says Varoth Chotpitayasunondh, a spokesman. The ministry is setting up a new reporting system to obtain official numbers faster. “We definitely cannot wait,” he says.




