To Mask, or Not to Mask Outside?
Warm weather is here and the voices are loud—it’s safe to be outdoors, and policy should reflect that. This week, outdoor transmission has dominated the conversation with news outlets big and small covering the relative safety of being outside—without a mask. Finally, on Tuesday, the CDC updated their guidelines to reflect that vaccinated people do not need to wear masks outdoors. Meanwhile, some cities and states continue to increase mask mandates, with Michigan extending theirs to young children.
In other news:
A dive into the data shows us that Florida is doing better than California---a discussion that’s been censored by YouTube; Len Cabrera walks us through it.
Sam Wald, speaking from his own family’s experience with 1930s Germany, warns us of the risk of dehumanizing people if we “other” them with vaccine passports.
Even over at the New York Times Ask Well columnist Tara Parker-Pope writes about the low transmission risk of going mask-free outdoors.
Heidi Tworek, et al., write in the Toronto Sun about the need for Canada to change its messaging about spending time outdoors.
Want to support our work? Visit our Substack page and leave us a tip.
COVID News
The CDC Finally Admits That Vaccinated People Don't Need Masks Outdoors
https://reason.com/2021/04/27/cdc-vaccines-outdoors-masks-walensky/
The Centers for Disease Control and Prevention (CDC) updated its public health guidance on Tuesday, finally conceding that people who are fully vaccinated do not need to wear masks while outdoors.
"There are many situations where fully vaccinated people do not need to wear masks," said CDC Director Rochelle Walensky, citing mounting evidence that the disease does not spread easily outdoors. "If you are fully vaccinated and want to attend a small outdoor gathering with people who are vaccinated or unvaccinated, the science shows, if you are vaccinated, you can do so safely unmasked."
Her remarks prompted a few reporters to ask why anyone has to wear a mask outdoors if COVID-19 is not easily spread under such circumstances, and whether vaccinated people wearing masks indoors was more about sending the right message than actually keeping people safe. In both of those cases, Walensky urged people to stick to the restrictions until more of the population is vaccinated and case rates have declined further.
Summer camp advice — keep masks and distancing — gets an update from the C.D.C.
https://www.nytimes.com/2021/04/25/health/covid-summercamp-cdc.html
Children going to camp this summer can be within three feet of peers in the same-group settings, but they must wear masks at all times, federal health officials say. The only times children should remove their masks is when they are swimming, napping, eating or drinking; they should be spaced far apart for these activities, positioned head to toe for naps and seated at least six feet apart for meals, snacks and water breaks.
The Centers for Disease Control and Prevention issued the anticipated updated guidance for summer camp operators this weekend, just weeks before many camps resume operations in mid-May. Many parents have been eager to find camps for their children, who had spent months indoors in remote learning classes during the pandemic.
A theme that runs throughout the updated guidance is the emphasis on conducting as many activities as possible outdoors, where the risk of infection in considered much lower than indoors. When activities must be brought indoors, spaces should be well-ventilated and windows should be kept open (windows should also be open on camp buses and vans), the C.D.C. said.
Should I wear a mask outside? Experts weigh in on scenarios.
https://www.washingtonpost.com/lifestyle/2021/04/22/face-mask-outdoor-wear-covid-safety/
As more Americans are vaccinated against the coronavirus and a growing body of scientific evidence suggests that the risk of outdoor transmission is low, many people are wondering: Do we need to keep wearing face masks outside?
The short answer is that masking outdoors can be “optional,” says Paul Sax, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital in Boston. While he says people should still generally don masks indoors, Sax believes statewide mandates for wearing masks outdoors may no longer be necessary. “The science of the viral transmission is advanced enough that we really don’t want to be kind of confusing people by forcing them to wear masks in places where really they’re at minimal risk,” he says.
But before you start spending all your time outdoors barefaced, Sax and other experts emphasize that decisions about when to wear a mask outside largely depend on personal risk assessments involving a variety of virus-related factors. What is your vaccination status? How many other people could you be interacting with? Do you know their vaccination status? How much prolonged close contact could you have with them? Are you, or is anyone in your household, at increased risk for becoming severely ill from covid-19?
We no longer need to fear covid
https://www.telegraph.co.uk/news/2021/04/24/no-longer-need-fear-covid/
The whole aim of practical politics, said HL Mencken, “is to keep the populace alarmed (and hence clamorous to be led to safety) by menacing it with an endless series of hobgoblins, all of them imaginary.”
It is hard to avoid the impression that officials are alarmed rather than pleased by the fading of the pandemic in Britain. They had a real hobgoblin to hand, and boy did they make the most of it, but it’s now turning into a pussy cat. So they are back to casting around for imaginary ones to justify their draconian – and deliciously popular – command and control over every detail of our lives. Look, variants!
And yes, the pandemic is fading fast. The vaccine is working “better than we could possibly have imagined”, according to Calum Semple, of the University of Liverpool, based on a study which found that it reduced hospitalisation by 98 per cent. With deaths from the virus now falling by more than 20 per cent a week and with overall mortality from all causes now below the long-term average, “we’ve moved from a pandemic to an endemic situation”, according to Sarah Walker, Professor of Medical Statistics and Epidemiology at Oxford and Chief Investigator on the ONS’s Covid-19 Infection Survey. The UK’s covid positivity rate at 0.2 per cent is now the fifth lowest in the world and lower than Taiwan and Israel.
Mark mandate goes into effect for kids ages 2 to 4 in Michigan
GRAND RAPIDS, Mich. — Beginning Monday, April 26, Michigan’s face mask mandate will also apply to children between the ages of two and four. That means they are now required to wear a mask in all public places, including schools, childcare centers and camps.
Earlier this month the Michigan Department of Health and Human Services extended the existing COVID-19 health order and added the new requirement.
“Even from the fall, the Centers for Disease Control and Prevention has said kids two and older should be wearing masks, to begin with. So, you know, this isn't an out of the blue, left-field kind of a thing that's being done now,” says Dr. Matthew Hornik, with Pediatric Care Corner in West Bloomfield Township.
Commentary/Analysis
Yes, the Covid mortality rate is higher in California than Florida
https://rationalground.com/yes-the-covid-mortality-rate-is-higher-in-california-than-florida/
Recently, Dr. Jay Bhattacharya wrote an opinion piece for the Wall Street Journal, critical of YouTube’s removal of the public-policy roundtable hosted by Florida Governor Ron DeSantis. In the opening paragraph, Dr. Bhattacharya stated an objective, verifiable fact that many people have trouble accepting: “Yet age-adjusted mortality is lower in Florida than in locked-down California, and Florida’s public schools are almost all open, while California’s aren’t.”
The term “age-adjusted mortality” may have people thinking that Dr. Bhattacharya is just making up statistics to tell his preferred narrative. Age-adjusted mortality makes Florida look better since it has the second-highest proportion of 65+ population in the country (20.9% compared to California’s 14.7%). Regardless of that fact, California has performed worse than Florida in terms of COVID-19 deaths in every way: total deaths, deaths per capita, and age-adjusted deaths per capita.
COVID-19 deaths are reported by the CDC in the table, ”Provisional COVID-19 Death Counts by Sex, Age, and State.” As of the April 14 update (data from Jan 1, 2020, to April 10, 2021), California’s total COVID deaths were 61,908, while Florida’s deaths were 31,564.
Discriminatory Passports – Never Again
https://rationalground.com/discriminatory-passports-never-again/
Americans are used to passports opening doors almost everywhere, so we view the documents like keys. We don’t have experience with passports that keep us out and that ostracize, marginalize, and dehumanize us. Now New York is introducing its own vaccine ID technology, and the Biden administration is working with companies to create a set of standards that will be used to introduce vaccine passports—or similar papers by other names—into multiple aspects of American life. Even without a federal mandate, a document that discriminates against and excludes a certain group of people from normal life activities is divisive and nefarious.
When my grandmother passed away at the end of 2020, a month shy of her 98th birthday, she left me her passport. This is not the indestructible blue book adorned with an American Eagle, but a faded and flimsy booklet from Austria, featuring a Nazi Eagle and swastika. The first page is stamped with a bright red J—for Jüdin, meant to mark her for the world as Jewish or, in that time and place, undesirable. This is not a passport that recognized her freedom to travel the world, as she later did as an American, but rather a document that separated her from others and designated her as unwanted and subhuman.
Do We Still Need to Keep Wearing Masks Outdoors?
https://www.nytimes.com/2021/04/22/well/live/covid-masks-outdoors.html
As more people get vaccinated and spring weather and sunshine beckon us outdoors, one question may be nagging at you: Do we still need to wear masks outside?
More than a year into pandemic life, many people remain confused about the risk of spending time outdoors around other people. A growing body of research shows that transmission of Covid-19 is far less likely outdoors than inside, and the risk will get even lower as more people get vaccinated and cases continue to decline. But many states have yet to lift strict outdoor mask mandates. In Massachusetts, for instance, outdoor masking is required at all times, even when nobody else is around.
Recently the online magazine Slate stirred controversy when it suggested an end to outdoor mask rules. The article won support from top public health experts and even The New England Journal of Medicine blog but prompted a fierce backlash from readers, who noted that while the risk of outdoor transmission may be low, it’s not zero.
Why we need to change the narrative on outdoor transmission
Last year, coming out of the first wave, many of us experienced a feeling of dread in May of 2020. We saw young people in Trinity Bellwoods park. They were not masking, not distancing and enjoying life as if there was no lockdown in place. Many of us were upset, feeling that the work over the past three months was lost.
But what happened? No transmission occurred, and Toronto’s cases hit an all-time low for the pandemic. We breathed a sigh of relief, learned and prioritized the outdoors. Playgrounds and parks that were closed were opened. Outdoor patios, sports and gatherings flourished. We learned in our quest to live with the virus that the outdoors offered a distinct advantage in significantly reducing transmission.
A year later, we still are talking about outdoor transmission. Yes, the emergence of the variants introduced a complicating feature, with increased infectivity and potential immune escape. Yes, case numbers in our communities are rising, with increasing health care utilization. Yes, vaccines are here, but not yet at a point where large-scale community protection has been achieved. However, none of these things has changed how the virus is fundamentally transmitted, through small droplets and aerosols. In other words, outdoor activity is generally safe whether there are 10 COVID cases a day or 10,000 — even with variants of concern.
Research
COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00790-X/fulltext
Background
BNT162b2 mRNA and ChAdOx1 nCOV-19 adenoviral vector vaccines have been rapidly rolled out in the UK from December, 2020. We aimed to determine the factors associated with vaccine coverage for both vaccines and documented the vaccine effectiveness of the BNT162b2 mRNA vaccine in a cohort of health-care workers undergoing regular asymptomatic testing.
Methods
The SIREN study is a prospective cohort study among staff (aged ≥18 years) working in publicly-funded hospitals in the UK. Participants were assigned into either the positive cohort (antibody positive or history of infection [indicated by previous positivity of antibody or PCR tests]) or the negative cohort (antibody negative with no previous positive test) at the beginning of the follow-up period. Baseline risk factors were collected at enrolment, symptom status was collected every 2 weeks, and vaccination status was collected through linkage to the National Immunisations Management System and questionnaires. Participants had fortnightly asymptomatic SARS-CoV-2 PCR testing and monthly antibody testing, and all tests (including symptomatic testing) outside SIREN were captured. Data cutoff for this analysis was Feb 5, 2021. The follow-up period was Dec 7, 2020, to Feb 5, 2021. The primary outcomes were vaccinated participants (binary ever vacinated variable; indicated by at least one vaccine dose recorded by at least one of the two vaccination data sources) for the vaccine coverage analysis and SARS-CoV-2 infection confirmed by a PCR test for the vaccine effectiveness analysis. We did a mixed-effect logistic regression analysis to identify factors associated with vaccine coverage. We used a piecewise exponential hazard mixed-effects model (shared frailty-type model) using a Poisson distribution to calculate hazard ratios to compare time-to-infection in unvaccinated and vaccinated participants and estimate the impact of the BNT162b2 vaccine on all PCR-positive infections (asymptomatic and symptomatic). This study is registered with ISRCTN, number ISRCTN11041050, and is ongoing.
Findings
23 324 participants from 104 sites (all in England) met the inclusion criteria for this analysis and were enrolled. Included participants had a median age of 46·1 years (IQR 36·0–54·1) and 19 692 (84%) were female; 8203 (35%) were assigned to the positive cohort at the start of the analysis period, and 15 121 (65%) assigned to the negative cohort. Total follow-up time was 2 calendar months and 1 106 905 person-days (396 318 vaccinated and 710 587 unvaccinated). Vaccine coverage was 89% on Feb 5, 2021, 94% of whom had BNT162b2 vaccine. Significantly lower coverage was associated with previous infection, gender, age, ethnicity, job role, and Index of Multiple Deprivation score. During follow-up, there were 977 new infections in the unvaccinated cohort, an incidence density of 14 infections per 10 000 person-days; the vaccinated cohort had 71 new infections 21 days or more after their first dose (incidence density of eight infections per 10 000 person-days) and nine infections 7 days after the second dose (incidence density four infections per 10 000 person-days). In the unvaccinated cohort, 543 (56%) participants had typical COVID-19 symptoms and 140 (14%) were asymptomatic on or 14 days before their PCR positive test date, compared with 29 (36%) with typical COVID-19 symptoms and 15 (19%) asymptomatic in the vaccinated cohort. A single dose of BNT162b2 vaccine showed vaccine effectiveness of 70% (95% CI 55–85) 21 days after first dose and 85% (74–96) 7 days after two doses in the study population.
Interpretation
Our findings show that the BNT162b2 vaccine can prevent both symptomatic and asymptomatic infection in working-age adults. This cohort was vaccinated when the dominant variant in circulation was B1.1.7 and shows effectiveness against this variant.
Funding
Public Health England, UK Department of Health and Social Care, and the National Institute for Health Research.
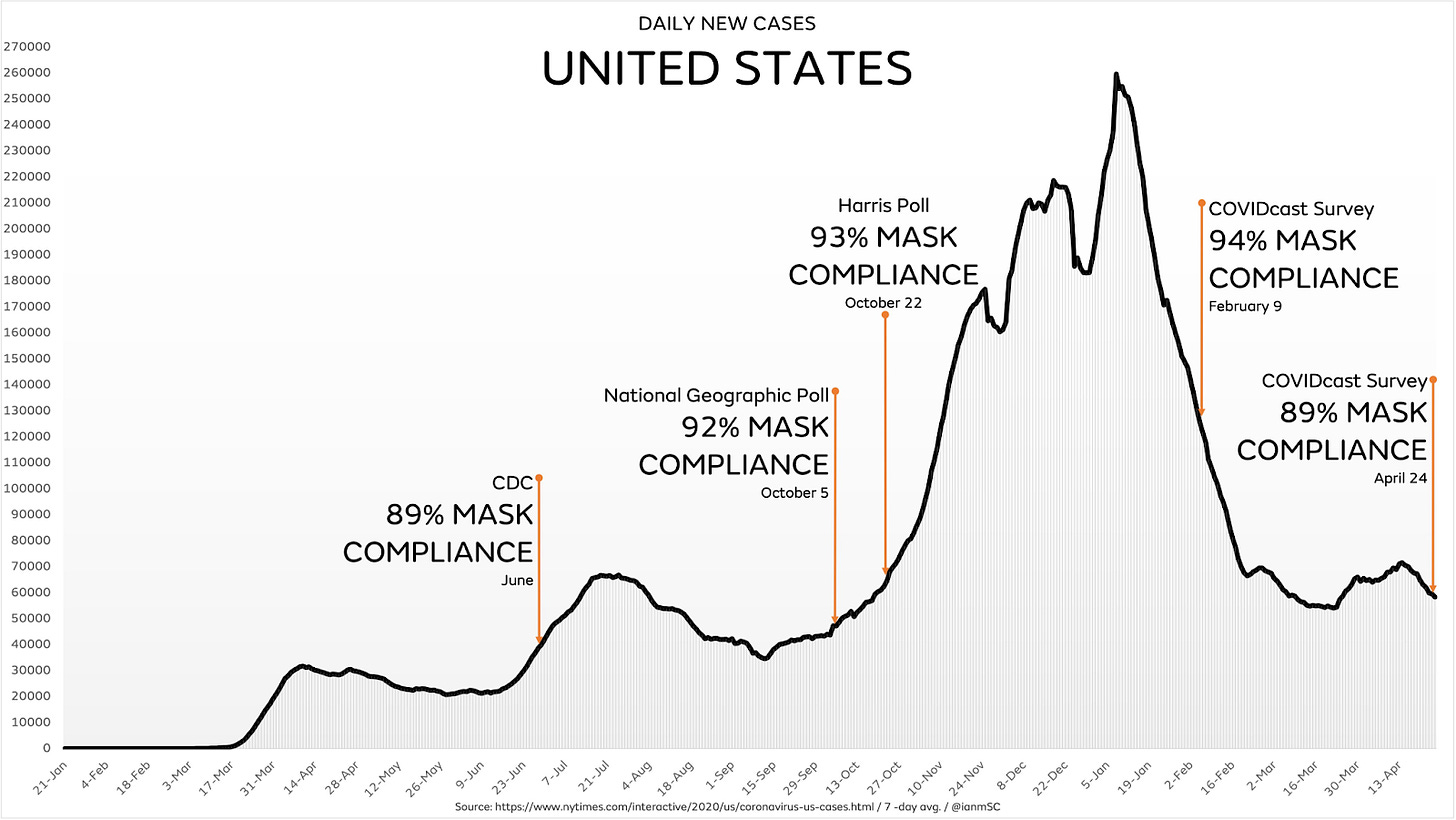
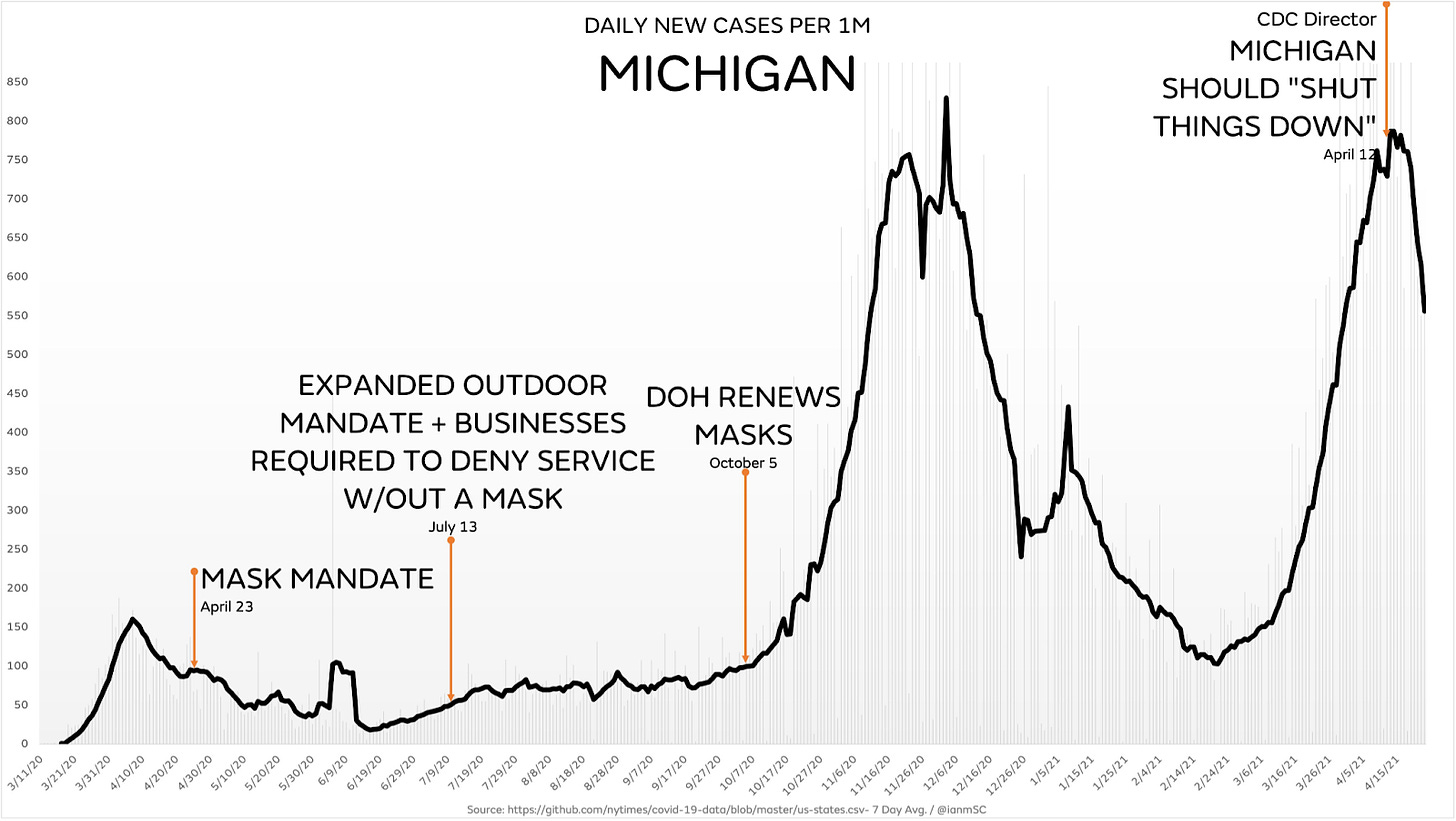
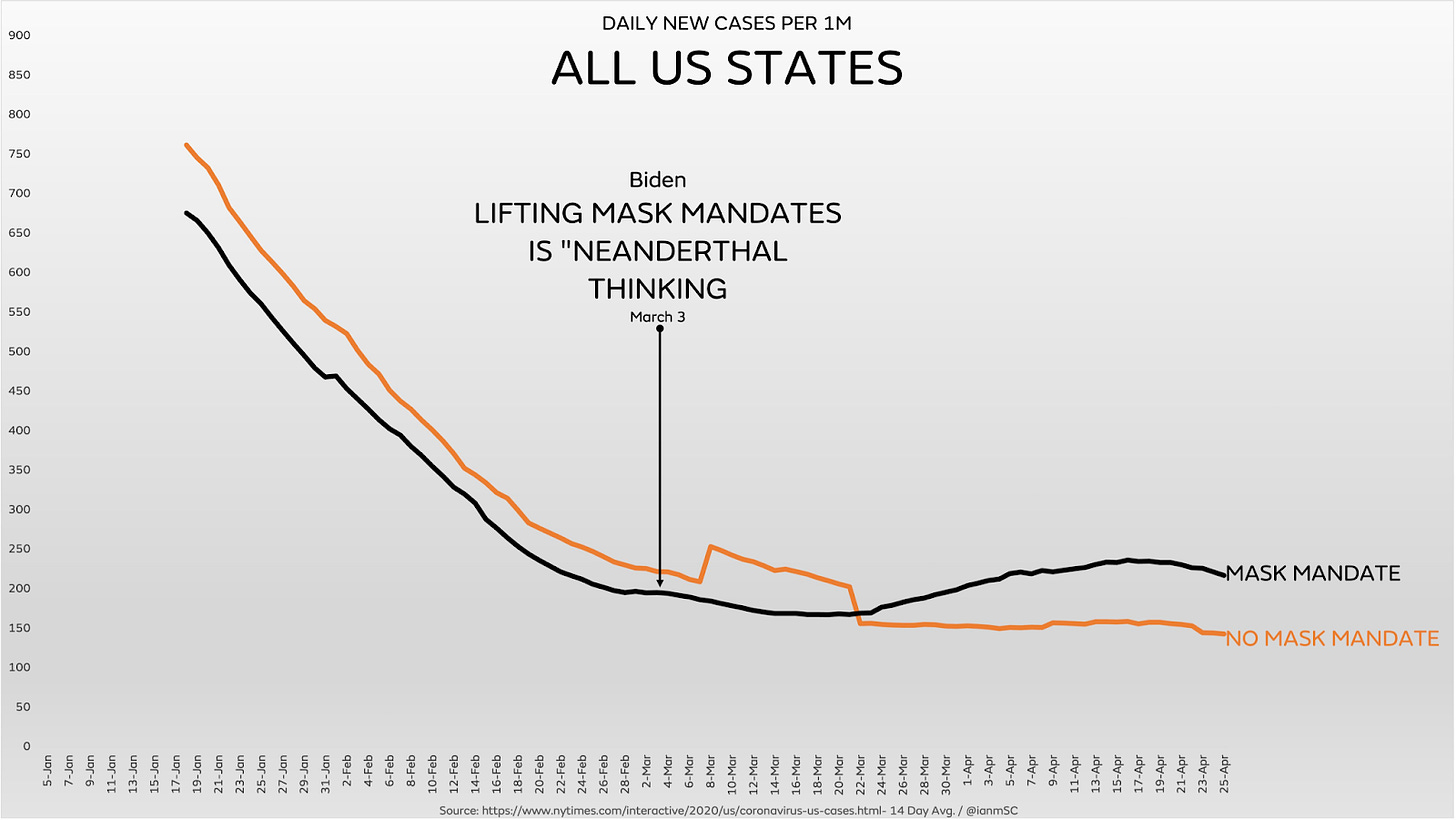
Charts and Graphics
International News
Israel records no new daily COVID deaths for first time in 10 months
https://www.timesofisrael.com/israel-reports-no-new-daily-covid-deaths-for-first-time-in-10-months/
For the first time in ten months, no new COVID-19 daily deaths were reported Thursday in Israel, according to the latest Health Ministry figures.
In data released Friday, the death toll remained unchanged from the day before at 6,346. The last date there were no new fatalities was June 29, when morbidity levels remained subdued following the initial coronavirus wave.
The ministry said of the 35,027 tests performed Thursday, 129 new cases were recorded, a positive test rate of 0.4 percent. The country has logged 837,870 confirmed infections since the pandemic began.