This is an oldie but goodie. Literally published 2 years ago and revised over time but still the only major non-institutional look at actual death certificates which I can tell.
From “Gone Viral: How Covid Drove the World Insane” - Chapter 7
… there was huge overstatement of the number of people hospitalized for Covid. By one estimate 50 percent of all Covid patients were in the hospital for something else entirely. Finally, there was a massive overcounting of Covid deaths based simply on a positive test result. In some states, deaths were counted as Covid deaths sixty days or even ninety days after recovery from Covid! If the person died within three months after a bout with Covid, well then, it was a fatality due to Covid.
This frightful wide net casting we discussed above hugely impacted morale across the country. As the pandemic waned in the spring of 2022, one report noted that 65 percent of all hospitalizations were incidental infections—people were in the hospital for something else, but because they tested positive for Covid, they were logged into the books as a Covid bed.
Now… look over the details here and ask yourself how this data fiasco can be stopped in the future!
Florida death certificate review raises questions about official number of COVID-19 deaths
BY JENNIFER CABRERA AND LEN CABRERA in conjunction with The Alachua Chronicle
There has been a great deal of debate over whether COVID-19 deaths are being counted correctly. Some people insist that they’re being undercounted, while others believe that they’re being overcounted.
We had the opportunity to review death certificates for some of Florida’s recent COVID-19 deaths, and we can tell you definitively that Florida is counting deaths that were not directly caused by COVID-19.
Public health agencies have a goal of tracking the spread of a reportable disease, and for that reason, guidance was issued in March that any person who tested positive for COVID-19 should be counted as a COVID-19 death. However, the death count is now prominently featured in newscasts and used as a talking point to claim that some governments aren’t “doing enough” to stop the spread of COVID-19. COVID-19 metrics, including the number of reported deaths, are increasingly cited by governments as a reason to write public health recommendations into law.
(Incidentally, a paper by the Institute for Pure and Applied Knowledge Public Health Policy Initiative claims the CDC did not submit a formal change proposal to the Federal Register before enacting the changes and did not allow a 60-day period for public comment and peer review, meaning that the Office of Management and Budget did not provide legal oversight, in violation of federal law.)
Specifically, some talking heads and media outlets blame every death in Florida on Governor DeSantis because he has not implemented draconian lockdowns and a statewide mask mandate. (Florida is ranked 11th in the United States in COVID-19 deaths per million; most of the top 10 are still under lockdowns, including the top two, New Jersey and New York.)
Review of reporting guidelines
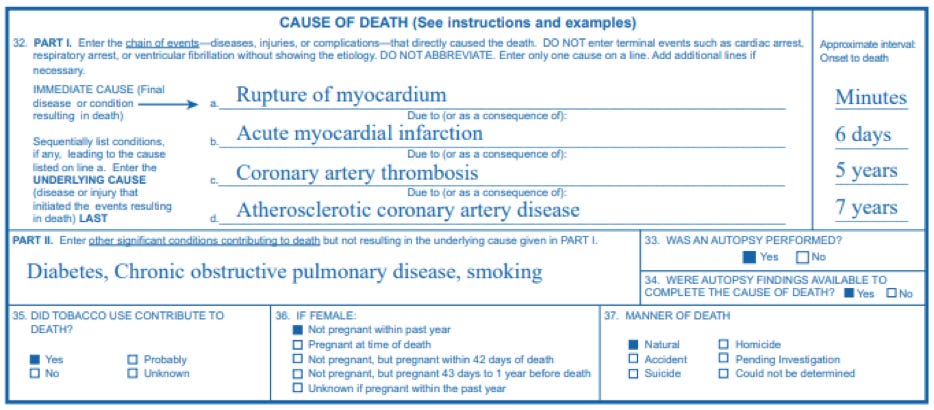
The Centers for Disease Control and Prevention (CDC) has a Physician’s Handbook on Medical Certification of Death that provides guidance to certifying physicians and medical examiners; the goal is that anyone not involved with the deceased or the event can read the report and clearly understand what led up to the death. The certificate has a clear “manner of death” by category (e.g., natural, homicide, accident, etc.). PART 1 should describe the chain of events that directly caused the death. Line a should be the immediate cause of death, followed by the events that result from the underlying cause, which is listed last. Here is an example from the CDC instructions:
Line a is considered the “mechanism of death,” but the CDC does not require listing a “terminal event” such as cardiac or respiratory arrest. PART 2 lists other significant contributing diseases or conditions that did not result in the underlying cause of death.
Florida House report on COVID deaths
Florida House Speaker Jose Oliva’s staff produced an Analysis of COVID Death Data report on October 12 that reviewed 13,920 death certificates provided by the Florida Department of Health on September 23. Of those records:
11,460 list COVID-19 as the immediate underlying cause of death in PART 1.
1,204 list COVID-19 as a cause, but not the underlying cause of death.
1,254 list COVID-19 as a condition in PART 2, but not a cause of death in PART 1.
2 did not list COVID-19 at all.
Of the 11,460 records that listed COVID-19 as the immediate cause of death, 8,058 (70%) listed no other causes. According to the report, these records were completed incorrectly, listing COVID-19 in Line a as the immediate cause of death rather than listing the result of COVID-19, such as pneumonia or acute respiratory disease syndrome (ARDS). While this does not imply the deaths were not caused by COVID-19, incorrectly-filled death certificates do not allow a clear distinction between deaths from COVID-19 and deaths with COVID-19.
Change in CDC guidance
A change in CDC guidance published on March 24, 2020 (COVID-19 Alert No.2) encouraged doctors to include COVID-19 in PART 1 “for all decedents where the disease caused or is assumed to have caused or contributed to death.” This was reinforced on April 5 (COVID-19 2020 Interim Case Definition), when the CDC said any death with COVID-19 on the death certificate is counted as a COVID-19 death, even if it was just presumed and had no confirming laboratory or clinical validation. In other words, the CDC guidance explicitly does not distinguish between deaths from COVID-19 and deaths with COVID-19.
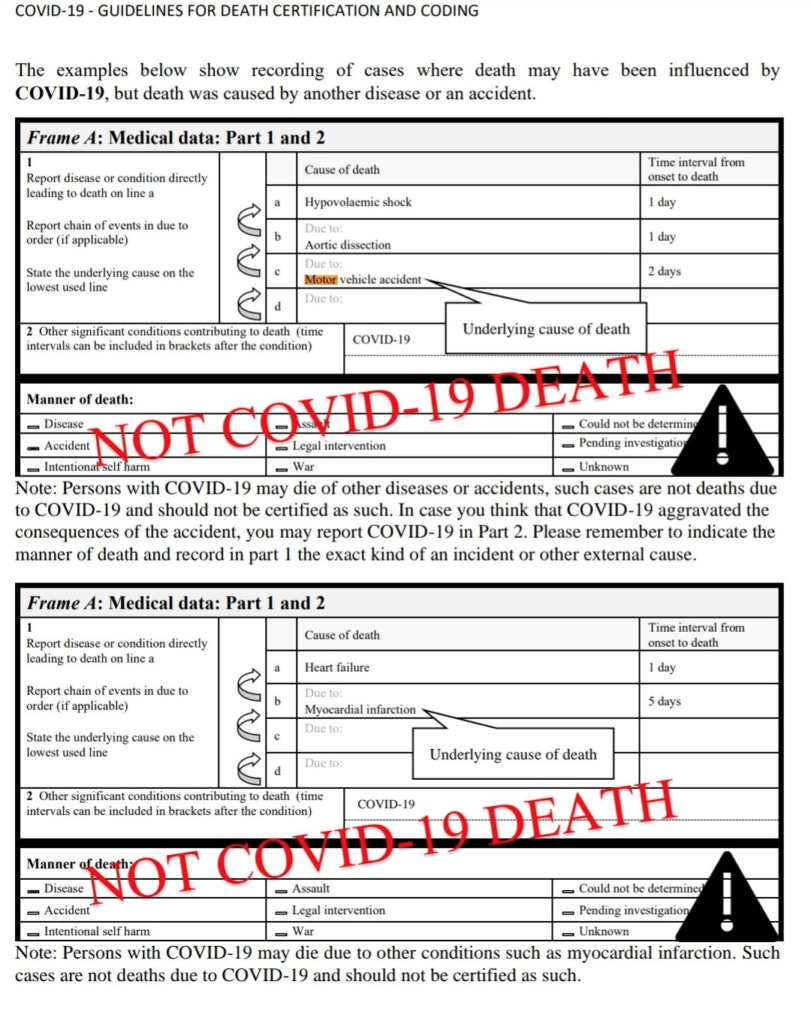
This is contrary to World Health Organization (WHO) guidelines, which say to count only deaths “resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma). There should be no period of complete recovery from COVID-19 between illness and death. A death due to COVID-19 may not be attributed to another disease (e.g. cancer).”
Unlike the CDC, the WHO specifies that COVID-19 listed in PART 2 is not considered a COVID-19 death. These examples are in their guidelines:
Our review of death certificates on October 22, 2020
We were provided with Florida’s COVID death certificates, but we only had a few hours to review them, so we started with a stack from September and October. We reviewed about 700 (heavily redacted) death certificates. Here is a summary of our findings:
About 15% were “lazy” (i.e., only listed COVID-19 on Line a, usually without any other entries in PART 1 or PART 2). It is highly unlikely that COVID-19 patients had no other conditions contributing to their death, especially for individuals aged 75 and older, who usually have multiple pre-existing medical conditions. Also, a typical progression for a COVID-19 death in PART 1 would look something like “a. Acute Respiratory Distress Syndrome b. Pneumonia c. COVID-19 infection,” with time intervals from onset to death for each line; few of the certificates we reviewed included these time intervals.
About a third were “interesting” because they either listed COVID-19 in PART 2 (i.e., death with COVID-19) or listed other significant conditions like renal failure, metastasized cancer, or strokes (i.e., people who would have probably died in the near future regardless of COVID-19). At least 5 of these were classified as accidents, not natural deaths.
About half we classified as “normal,” meaning they at least listed pneumonia along with COVID-19, even if they did so on the same line in PART 1 and left PART 2 blank.
Over half left PART 2 blank. With a median age of 76 and 81% aged 65 or older, it is highly unlikely that there were no other significant health conditions. The certificates that did not leave PART 2 blank had an average of 3 co-morbidities.
About 10% of the “interesting” death certificates listed some form of “Adult failure to thrive” or malnutrition. We don’t know how typical this is for elderly death certificates, but it may be related to the isolation imposed on long-term care residents during COVID-19.
Although a few certifying doctors made it clear that they thought the COVID-19 test was incidental (at best) to the death by writing things like “Asymptomatic positive COVID-19 swab” or “COVID-19 6 months ago,” these deaths were still counted as COVID-19 deaths.
Examples
Here are some examples of death certificates that were counted as COVID-19 deaths in Florida (each line starts with the age and gender of the decedent; manner of death is “natural” unless otherwise noted). These are not a representative sample, just some of the ones we found “interesting”:
84M, PART 1: a. Cerebrovascular accident, b. atherosclerosis, PART 2: COVID-19 pneumonia
85M, PART 1: a. Ischemic cardiomyopathy, PART 2: Chronic kidney disease, COVID-19
57M, PART 1: a. Coronary artery disease, PART 2: asymptomatic COVID-19 positive swab
88M, PART 1: a. Failure to thrive, b. dementia, c. type II diabetes, PART 2: COVID-19 positive
79F, PART 1: a. renal cancer – 4 months, PART 2: COVID-19
56F, PART 1: a. complications of paraplegia (non-traumatic), PART 2: Chronic obstructive pulmonary disease, diabetes mellitus, COVID-19
77F, Accident, PART 1: a. exacerbation of COVID-19 pneumonia, b. prolonged bed rest, c. left femoral neck and pelvic fracture, d. fall, PART 2: fall from standing height
96M, PART 1: a. hypertensive cardiovascular disease, PART 2: renal insufficiency, anemia, COVID-19
59M, PART 1: a. cardiorespiratory arrest, b. failure to thrive, c. developmental delay, PART 2: COVID-19, urosepsis
90F, PART 1: a. cardiopulmonary arrest 2nd to arrhythmia, b. failure to thrive, c. recovered from COVID-19, PART 2: dementia, HTN, hypothyroid
98F, PART 1: a. Cerebral atherosclerosis, b. vascular dementia without, c. behavioral disturbances, d. COVID-19 positive, PART 2: chronic fatigue, respiratory distress
74F, Accident, PART 1: a. COVID-19 infection & bronchopulmonary aspergillosis complicating sequelae of blunt force injury of right, PART 2: diabetes, hypertension, cardiovascular disease, obesity
84F, PART 1: a. Alzheimer’s, PART 2: COVID-19 disease
88M, PART 1: a. cancer of larynx, PART 2: COVID-19 infection
85F, PART 1: a. Arteriosclerotic CV disease, PART 2: Atrial fibrillation, COVID-19
41M, PART 1: a. Cardiac arrest – immediate b. Respiratory failure, acute on [sic] chronic – days c. Pulmonary artery hypertension – years d. Sarcoidosis – years, PART 2: COVID-19
69M, PART 1: a. Multiple ischemic strokes, PART 2: Chronic renal failure, recent COVID-19 pneu, dementia
70M, PART 1: a. Natural causes – years, PART 2: Neurocognitive (congenital developmental) delay, COVID-19 infection, recurrent aspiration pneumonia
60M, PART 1: a. Septic shock – days b. E Coli Bacterium-UTI c. GI bleed – acute blood loss anemia-esophageal necrosis d. acute hypoxemic respiratory failure, PART 2: Hypertension, HX of COVID
88F, PART 1: a. Complications of dementia, PART 2: Atrial fibrillation, arteriosclerotic cardiovascular disease, COVID-19
79F, PART 1: a. Coronary artery disease – years, PART 2: COVID-19, myeloproliferative disorder, diabetes, Parkinson’s
83F, Accident, PART 1: a. Complications of COVID-19 – NS, PART 2: Traumatic brain injury, failure to thrive, atherosclerotic and hypertensive cardiovascular disease, urinary tract infection
87F, PART 1: a. Senile degeneration of brain, PART 2: Complications related to COVID-19 infection
98F, PART 1: a. End stage dementia b. Adult failure to thrive c. Positive COVID-19, PART 2: blank
64M, PART 1: a. Acute heart failure b. Chronic systolic heart failure c. Ischemic cardiomyopathy d. A. Fib, hypertension, HLD, PART 2: COVID-19
72M, PART 1: a. Parkinson’s disease, PART 2: Hypertension, history of COVID-19 and deep vein thrombosis in July
89M, PART 1: a. Cardiorespiratory arrest b. Failure to thrive c. Arteriosclerosis cardiovascular disease, PART 2: COVID-19
82F, PART 1: a. Unknown b. Failure to thrive, depression – 7 days c. Exposure to COVID-19, cough and shortness of breath – 14 days d. Dementia, hypothyroidism, atrial fibrillation, bronchospasm, congestive heart failure – years, PART 2: History of refusing medications and food for at least 7 days, refusal to go to the emergency room
77M, PART 1: a. Stage 4 small cell carcinoma of the lung, PART 2: COPD, COVID-19 pneumonia, hypertension
61M, PART 1: a. Metastasis to liver of unknown origin b. Adenocarcinoma c. COVID-19 d. Severe protein-calorie malnutrition, PART 2: blank
69F, PART 1: a. Glioblastoma – months, PART 2: COVID-19 pneu
78F, PART 1: a. End stage Parkinson’s disease, PART 2: COVID-19 pneu, HTN, CAD
83M, PART 1: a. Dementia b. Parkinson’s c. B Cell chronic lymphocytic leukemia d. CKD-III, PART 2: COVID-19
81F, PART 1: a. Small bowel obstruction – weeks, PART 2: CHF, renal failure, dementia, COVID-19
62M, PART 1: a. Severe sepsis due to obstructive pneumonia – 5 days b. right lung mass, likely cancer – 60 days, PART 2: Acute renal failure, brain metastasis, COVID-19 infection
90F, PART 1: a. complications of dementia, PART 2: Arteriosclerotic cardiovascular disease, COVID-19
76M, PART 1: a. Cardiorespiratory arrest b. End stage renal disease in hemodialysis c. insulin dependent diabetes mellitus, PART 2: Cerebrovascular accident, HTN, hyperlipidemia schizophrenia necrotic sacululcar [sic] COVID-19 infection
72M, PART 1: a. Esophageal adenocarcinoma with lung and liver metastases, PART 2: COVID-19 pneumonia
57M, PART 1: a. Myocardial infarction, PART 2: COVID-19 infection
75M, PART 1: a. End stage ALS, PART 2: Respiratory failure secondary to COVID-19
94F, PART 1: a. Arteriosclerotic cardiovascular disease, PART 2: Hypertension, dementia, COVID-19
90F, PART 1: a. Cerebrovascular accident b. Atrial fibrillation, PART 2: COVID (6/2020)
87M, PART 1: a. Cardiorespiratory arrest b. dilated cardiomyopathy c. aortic insufficiency/secondary to AV block d. COPD, PART 2: Parkinson’s, vascular dementia, duodenal ulcer, H/O COVID+
92F, PART 1: a. Sequelae of femoral neck fracture b. Blunt impact to extremity, PART 2: Asymptomatic COVID-19 infection, hypertensive heart disease
65M, PART 1: a. Complications of hepatocellular carcinoma, PART 2: Obesity, COPD, COVID-19, hypertension
69F, PART 1: a. Complications of urinary tract infection, PART 2: Chronic ethanolism, COVID-19, hypertension, diabetes mellitus
92F, PART 1: a. Sepsis b. Multidrug resistant bacteremia, PART 2: Decubital wound, COVID-19, dementia, chronic kidney disease stage III, hypertension, diabetes mellitus type II, hyperlipidemia
94M, PART 1: a. Multiple diseases of the elderly, PART 2: Cerebrovascular disease, vascular dementia, hypertension, chronic lymphocytic leukemia, atrial fibrillation, COVID positivity
88M, PART 1: a. Multiple diseases of the elderly, PART 2: Cerebrovascular disease with previous strokes, vascular dementia, COVID-19 positivity, hypertension
61M, PART 1: a. Hepatocellular carcinoma, Hepatitis C, PART 2: COVID-19, non-small cell lung cancer, cirrhosis
97F, Accident, PART 1: a. Complications of right intertrochanteric femur fracture, PART 2: Hypertensive and arteriosclerotic cardiovascular disease with congestive heart failure, complications of COVID-19
52F, PART 1: a. Liver failure b. Metastatic disease c. Breast cancer, PART 2: Coagulopathy, septic shock, COVID-19
80M, PART 1: a. Dementia b. Cerebrovascular disease c. COPD d. Coronary artery disease, PART 2: C19+
90M, PART 1: a. Octogenarian natural causes b. S/P C19, PART 2: blank
97M, PART 1: a. Complications of dementia, PART 2: CKD, COVID-19, Protein calorie malnutrition, Arteriosclerotic cardiovascular disease
60F, PART 1: a. Intracranial bleed b. End stage liver disease, PART 2: Pneu, COVID-19 positive history, hypertension, cirrhosis, anemia
89F, Accident, PART 1: a. Complications of hip fracture, PART 2: Cerebrovascular accident, Arteriosclerotic and hypertensive cardiovascular disease, dementia, COVID-19
91F, PART 1: a. Left hip ORIF repair b. COVID + history c. CABG X 4 vessels d. Heart failure, PART 2: COPD
(original publish date: 11/11/2020)




Along the same lines, you can go through a database of covid-assigned deaths from Florida's medical examiner. The database stopped being updated in August 2020. Its chronicles are similar to the certificates the Cabreras went over. It's at https://www.floridatoday.com/story/news/2020/07/11/update-searchable-florida-medical-examiners-database/5415936002/
thanks for this analysis. Why were you given only a couple of hours to review these certificates? That's a red flag right there.